30 March 2020
A roundup of some of the most interesting things I’ve read in the last few days.
Tomas Pueyo, who authored the highly influential (and highly recommended) post, “Why you must act now” back on 10 March, has published a sequel, “The Hammer and the Dance.” His summary:
Strong coronavirus measures today should only last a few weeks, there shouldn’t be a big peak of infections afterwards, and it can all be done for a reasonable cost to society, saving millions of lives along the way. If we don’t take these measures, tens of millions will be infected, many will die, along with anybody else that requires intensive care, because the healthcare system will have collapsed.
It covers some of the same ground as the early piece, but is well worth reading.
Tomas’s article led me to the impressive, interactive Epidemic Calculator. If you take only one thing away from using it, it’s that outcomes are wildly sensitive to inputs that are difficult to estimate.
This very good FT piece (paywall, but this link in theory should let you read it), The mystery of the true coronavirus death rate, covers several important topics. As the title suggests, it discusses with the Case Fatality Ratios (CFRs) have been so different in different countries, and why we should be cautious about comparing them. (See my discussion here.). It covers the thorny question of many deaths from coronavirus are indeed incremental. And it helpfully reminds us that with testing rates so wildly different by country, we really don’t have a good sense of the true rate of infection, and therefore don’t know the true Infection Fatality Ratio.
An extremely important study came out of Iceland lately, discussed here. It is perhaps the highest rate of testing (per capita) in the world of a country testing a significant portion of the population; and importantly, it screened the general population, not just symptomatic or at-risk individuals.
The updated figures are here, on a Government of Iceland website.
According to numbers published by the government on Wednesday 25 March, a total of 11 727 individuals have been tested for the virus that causes COVID-19. This translates to 32 217 on a per million basis. This is the highest proportion of tests performed by any individual country.
So they’ve tested around 3% of the population.
Importantly, two very different cohorts were tested: one representing the general population, and one focused on symptomatic or high-risk patients.
The tests have been performed on two different cohorts.
A total of 5 564 tests have been performed by the National University hospital of Iceland in Reykjavík, mostly on individuals who were symptomatic or were considered to be likely to have contracted the virus due to proximity to infected individuals or other reasons. Out of these 5 564 tests, 4 879 have been negative and 685 positive.
A total of 6 163 tests have been performed on the general population, individuals who had not been ordered to quarantine and were generally asymptomatic or showed mild symptoms. Out of these 6 163 tests, 6 111 have been negative and 52 positive.
So 12% of the symptomatic/high-risk patients were positive; but only 0.8% of the general population.
While Iceland is different in so many ways from many other countries, this is at least one data point that argues against the idea that a very high portion of the population might already have been infected, with an extremely low rate becoming ill, critically ill, or dying.
A meta-point to take away from it is that when you see reports about the distribution of confirmed cases by age group, you should first ask yourself whether the sample is random or suffers from extreme selection bias. As one Dutch professor tweeted:
It’s possible that the elderly in the Netherlands are many times more likely to get ill than those in Iceland, and that young Dutch are uniquely immune. But it’s much more likely that this reflects a combination of selection bias in the testing, and the fact that younger people are more likely to have mild cases and not go for testing.
This tool, comparing hospital resources (capacity) to projected critical cases for the US, both at a national and state level, is making the rounds quite broadly.

I haven’t looked at the methodology yet to see what caveats to attach to it, but have seen some sniping from individual states who believe it is inaccurate for their state.
The Harvard epidemiologist, Marc Lipsitch, at the Center for Communicable Disease Dynamics, wrote a very important tweet which I recommend you read in full: https://mobile.twitter.com/mlipsitch/status/1243347447537115136.
The key point is that while we should do everything we can to control the spread of the virus, he is pessimistic that we will be able to avoid a high (>20%) attack rate.
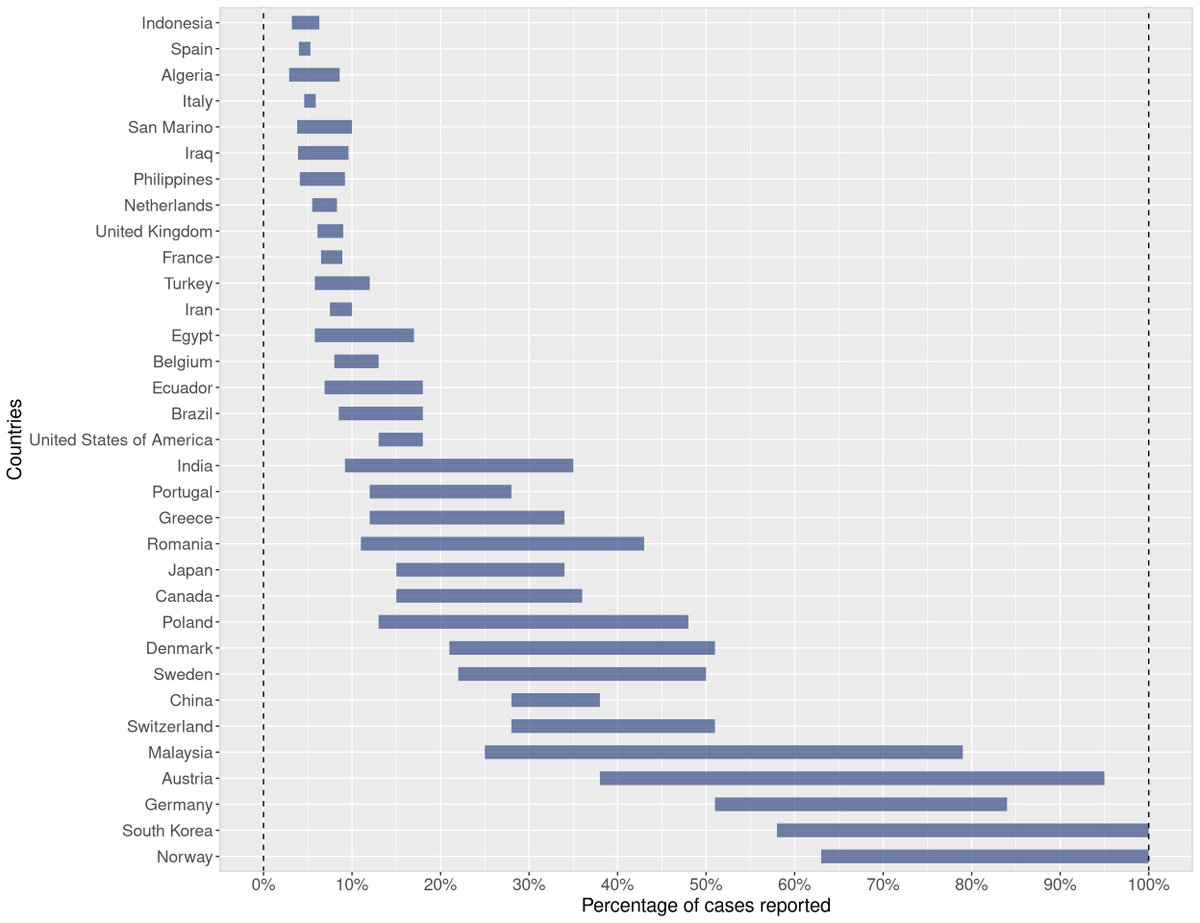
A study estimating the degree of underreporting I quoted in another post has been updated. I’ve updated it there; here is the latest: